Hixny’s participation in the NCQA Data Aggregator Validation process, now in its fourth year, showed one payer how access to reliable data at scale improved their reporting of quality measures.
For Capital District Physicians’ Health Plan, Inc. (CDPHP®), HEDIS reporting has always been an area of focus. The health plan’s longstanding, proactive approach to gathering data from patient records is well-known among participating providers. And although plan analysts expected to gain efficiency by using Hixny’s NCQA-validated data, they were shocked to find they gained accuracy and improved their capture of provider performance against critical HEDIS quality measures, too.
“I’m coming up on 10 years at CDPHP, and every year we’ve been looking at more than 30 supplemental data sources for HEDIS reporting,” says Suzanne Beck, CDPHP principal quality health care analyst. “We’ve been taking on one provider installation at a time, as finding time for physician offices to focus on something other than providing clinical care is difficult, nor is it always easy to understand the data we are looking for. It’s a heavy process burden on CDPHP and on providers. And it’s not scalable.”
The benefit of the NCQA Data Aggregator Validation (DAV) program to CDPHP is that the quality of the data is checked on the input side, so the health plan can be confident in the data it is extracting for reporting purposes.
Why does more data matter?
Beck and her colleagues never expected that pre-validated data at scale would significantly shift the CDPHP understanding of provider effectiveness and the quality of patient care its members receive. Yet that’s exactly what happened during the 2023 HEDIS reporting season.
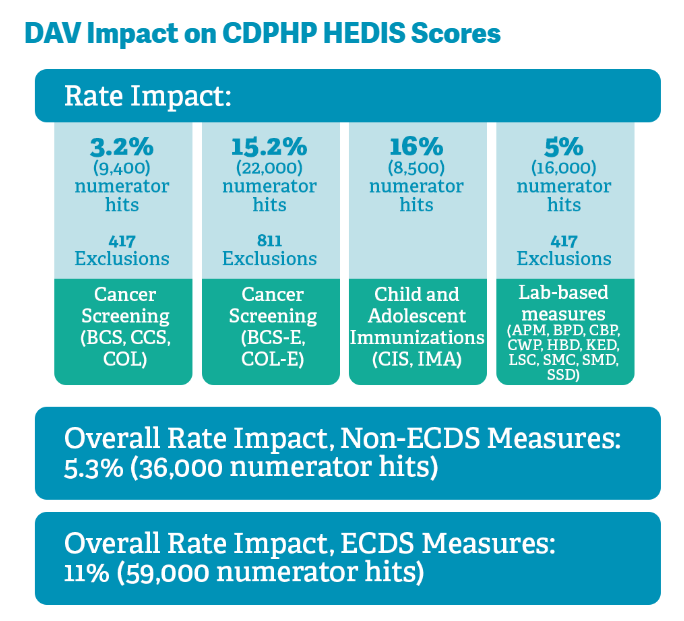
“We were already achieving high results because closing gaps is a priority for CDPHP. But when we saw the data, some things really stood out,” she explains.
- 7% more short-term follow-ups for newly initiated care were reported, from a baseline of 40%
- 4% more flu vaccines showed through Hixny than were previously known from pharmacy claims—and reported childhood immunizations increased, too
- 12% more patients were reported as having controlled high blood pressure—which rose to 14% more among patients who also had diabetes
Among cancer screening reports:
- Breast cancer screening rose 19% with 125 exclusions identified
- Colon cancer screening rose 12% with 682 exclusions identified
- Cervical cancer screening rose 3% with 375 exclusions identified
“The exclusions are perhaps even more important than the reports of screening,” Beck points out. “If we know someone has a condition that excludes them from screening, it helps ensure the accuracy of the data and reduces excess provider work. It also really helps us avoid member abrasion by preventing inappropriate conversations—like asking someone who has had a preventive mastectomy why they haven’t had a mammogram this year.”
Efficiency is a big win
Where CDPHP doesn’t see data through Hixny, Beck’s team reaches out to provider groups individually or works with Hixny to encourage the groups to provide their data and to participate in the NCQA DAV process.
“We’re working on a dashboard that will let us look at what provider groups are making their data available through Hixny,” Beck says. “Where there is good coverage at the PCP or specialty level through Hixny, we don’t need to work with them to set up a separate process. We can get the data through Hixny with a fraction of the effort it took to retrieve data directly.”
Payers who have not had robust IT support or who have been less proactive than CDPHP about gathering information from supplemental sources could realize impact rates even higher than those that CDPHP reports, Beck estimates.
Looking toward the horizon
“We see a lot of proprietary codes in data sets,” Beck begins, as she reflects on the next steps in the CDPHP use of Hixny for HEDIS reporting. “We’re starting to map those codes to HEDIS-acceptable codes to reflect specific tests and such.”
The health plan is also working to educate patients about the benefits of consenting to their providers sharing information through Hixny. At the same time, Beck and her team are helping providers to recognize Hixny fills in the blanks in reporting that inevitably appear when clinical and claims data aren’t aligned.
“New York State has been very aggressive in asking us to capture depression screenings and social determinants of health, and Hixny is able to help there, too,” Beck explains. “Any area where we can’t use claims data alone is a focus for us going forward.”


