Dr. Adetutu Adetona, Lansingburgh Family Practice
Most healthcare offices operate according to systems and habits. Providers and their teams are used to doing things a certain way and often, if asked, “Why do we do it this way?” they answer, “Because that’s the way we’ve always done it.”
Now, though, healthcare professionals throughout New York and the country don’t have any choice but to change the way they work. As the evolving federal incentive model approaches its 2020 rollout, providers and organizations are being led—or dragged—into the future.
At the heart of this seismic shift in the healthcare landscape is value-based care, a delivery and payment model that focuses on quality and efficiency rather than quantity. Its implementation is forcing providers to change the way they think, act and use information. The expectation is that transforming the relationship between the payer, provider and patient will help control healthcare costs while improving outcomes.
In the value-based care model, providers take on the responsibility of ensuring that their patients receive all the services they need to produce the best results. The idea is to leverage connections, communication and data to maximize efficiency and spend more time with patients. This may mean forming a risk-bearing entity such as a patient-centered medical home (PCMH), accountable care organization (ACO) or health home. Providers are evaluated based on quality metrics. Those who deliver on the promise of improving patient experience and outcomes, while lowering costs, often receive more in compensation than they would under the traditional fee-for-service model.
Making the Model Work
Dr. Adetutu Adetona may not seem a likely candidate for success in this changing world. She is a solo practitioner with three employees in an underprivileged upstate community. She also, by her own admission, is not particularly computer savvy.
Adetona opened her Lansingburgh Family Practice more than 20 years ago, after moving to the United States from Nigeria in 1995. Her goal was to make a difference and use her skills to serve a population in need. Today, her practice has about 2,000 active patients, 85 percent of whom are on Medicaid or Medicare.
She saw the focus beginning to shift from quantity to quality of care years ago. In fact, Adetona held a deeply rooted belief that patient outcomes are the most important measurement—not how many tests, labs and medications she could order and bill. Instinctively, she knew she’d need quick access to data about her patients so she could use this information to improve outcomes.
Her practice location dictated that most of her patients’ urgent care needs were met at the St. Mary’s Hospital or Samaritan Hospital emergency departments (EDs). When she met with patients for ED follow-ups, she and her staff worked diligently to get the proper records from each hospital. Sometimes the information was available through their electronic health record (EHR) system, but most of the time, one of her staff members had to call and request this information. The records came back by fax, usually after the visit was over. If information in the records wouldn’t have changed her diagnoses or recommendations, the records were simply added to the patient’s paper file. If the information was unusual, her staff would reach out to the patient to schedule an appointment so they could take the appropriate action.
Adetona knew there had to be a better way. As a provider working with Capital District Physicians’ Health Plan (CDPHP), she learned of a new program based on patient outcomes. CDPHP’s Enhanced Primary Care (EPC) program began in 2008 with the goal of rewarding providers for value-based care.
The program, which is based on the PCMH model, was also intended to address the shortage of primary care doctors by relieving them of fee-for-service systems and empowering them to support their patients. EPC providers transformed how they practiced—using EHRs, coordinating with other professionals on patients’ care teams, extending office hours, leaving time available for same-day appointments, communicating with patients by text or email and giving the greatest attention to the patients with the most needs. In turn, they were compensated based on a broad set of performance measures, including cancer screening rates, medication management and diabetes control, among others.
The EPC program was one of the first of its kind in the nation. In creating it, CDPHP recognized that, to lower healthcare costs, healthcare professionals needed to work more efficiently—while improving population health and patient satisfaction. In other words, providers needed to be able to balance all three goals of the “triple aim.”
The national recognition began early. In 2012, two CDPHP leaders spoke about the program at a national conference and before a subcommittee of the U.S. House of Representatives in Washington, D.C.
“Sometimes people stand at the base of a mountain and look up to the top and say to themselves, ‘How am I ever going to get up there?’” explained Dr. John Bennett, CDPHP President and CEO. “Instead of looking up, we looked down and agreed that we were going to take it one step at a time.”
The New York State Department of Health is using initiatives such as the Delivery System Reform Incentive Payment (DSRIP) program to shift 80 to 90 percent of Medicaid managed care reimbursement to value-based payments by 2020.
As for Adetona, she was always conscious of her performance, using claims data from insurers to monitor her progress and making corrections she thought would improve the care she provided. And yet, when CDPHP approached her about the EPC program, she was wary.
“It was a fear of the unknown,” she said. “I was comfortable with fee-for-service. I improved what I needed to improve. I saw no advantage in changing. That’s the honest truth.”
But she also knew she had little choice but to embrace the future. Value-based care was already entering the mainstream and would continue to make inroads as payers and regulators pushed for better outcomes and lower costs.
The shift has accelerated in recent years thanks to federal initiatives such as The Medicare Access and CHIP Reauthorization Act (MACRA) and incentive programs established under the Affordable Care Act (ACA). The New York State Department of Health is using initiatives such as the Delivery System Reform Incentive Payment (DSRIP) program to shift 80 to 90 percent of Medicaid managed care reimbursement to value-based payments by 2020.
The movement has put pressure on providers to think and work differently, to form new relationships with their colleagues, to embrace EHRs and to increase their reliance on vital, real-time patient data like that offered by Hixny.
How One Practice Succeeded
“In the beginning we struggled, but I was determined,” laughed Adetona, who said the biggest change was not in how she delivered care, but the way she accessed and collected data.
“The first patient took me almost two hours to find all the necessary records and input them, but I wasn’t going to quit,” she said. “In those early days, my waiting room was full and I would come out and apologize and tell my patients it was a new system and ask for their patience. Now they laugh and say, ‘Remember when … ?’ It shows the journey I took.”
Adetona took that journey one small step at a time, easing her staff along with her. She said that by exuding confidence—even when she didn’t always feel it—she gave them confidence. Now that everyone in her practice is comfortable with electronic data, she explained, “it makes our job so much easier.”
For her, it’s not just about efficiency, but improving patient care by supporting—not replacing—the human element. She believes that her personal involvement with each patient is the most important element of care and one of the keys to her success. And Hixny helps in that regard.
At the end of each day, the practice pulls continuity of care documents (CCDs) for every patient whose Hixny consent is on file—about 90 percent of them—and who is scheduled to come in the next day. That way, the team is prepared to speak to the patient from a shared base of knowledge.
For example, when a patient checks in, the receptionist can see that he or she didn’t get the test Adetona ordered during the last visit, and so can ask the patient about this and make a note. Then, when the patient enters the exam room, the medical assistant can look at the record and confirm that the patient didn’t get the test. “By the time I come in, the patient knows I know they didn’t follow through with my orders. We discuss it and I find out why—and then ensure they will get that test, soon. It’s a team effort.”
This approach allows Adetona to be even more engaged with her patients. Now, when speaking with them, she enters the information into the EHR, instead of trying to look up older records. If the patient doesn’t have certain information, she checks the Hixny CCD or pulls an additional record.
“All you need to do is hit a button and the test is right there. I can find it through Hixny.” —Dr. Adetutu Adetona
“You don’t know what test they had? All you need to do is hit a button and the test is right there,” she said. “You want to know what pharmacy they use? The doctors they’ve seen? It’s all there. Sometimes a patient will say they had a ‘very high’ blood pressure reading at the ED, but they don’t know what it was. I can find it through Hixny.”
This means that everyone on Adetona’s team is accessing real-time data through Hixny’s health information exchange (HIE) and reinforcing her direction, all the way through the patient’s departure from the visit. The team’s personal, hands-on approach has paid dividends.
Through her dedication to improving workflow, Adetona has earned the top ranking for quality and effectiveness among more than 200 practices in CDPHP’s EPC program. Her EPC quality score of 97.5 percent is well above the program average of 76.5 percent.
Bennett said Adetona has succeeded “because she believes in it. She’s a very hard worker. She’s passionate about her patients and she loves what she does.”
In addition to being a top performer in the EPC program, Adetona is ahead of her peers when it comes to accessing records within Hixny. Adetona was honored, along with her EHR vendor MEDENT, as game changers by Hixny in 2012. That year Mark McKinney, CEO of Hixny, awarded her for her early adoption and for being a pioneer in contributing data and accessing electronic health records. “We recognized Dr. Adetona years ago for her understanding of the role Hixny could have through electronic health information to support her in providing better care coordination. Through her hard work and dedication, we are pleased, but certainly not surprised, that she is leading the way in the EPC program. The results prove it. Utilizing Hixny and incorporating the HIE into her daily workflow is undeniably improving the care of her population, increasing patient satisfaction and lowering healthcare costs.”
“Dr. Adetona is a leader in the region when it comes to accessing available information within Hixny. She utilizes Hixny every day, for every single record, for every single patient,” stated McKinney. “Records are automatically pushed to her staff as they get ready for the day ahead, and as needed they ‘pull’ records from the HIE. She is a model of efficiency within our region.”
“Hixny bridges the gap. It gives you a global picture of what has happened with your patient outside your office,” Adetona said. “If you’re going to deliver good healthcare, you really need to know who your patients are seeing, what medications they’re taking, what tests they’ve had done. When someone comes into my office I have their CCD on my screen and I can see all of that. That’s one way Hixny helps me.”
 Dr. Adetona speaks with a patient at her Troy office where she has been practicing for more than 20 years.
Dr. Adetona speaks with a patient at her Troy office where she has been practicing for more than 20 years.
Value-based care requires efficiency, and Adetona said that by tapping Hixny as a resource, instead of calling or faxing for information, her staff is “saving hours in the day’s workflow, and in any practice that makes a major difference.”
With the patient’s information at her fingertips, Adetona can make medical decisions and order tests or medications while she’s with the patient.
What’s the Bottom Line?
There is evidence that value-based care works. According to data from the Centers for Medicare and Medicaid Services, Medicare ACOs saved more than $460 million in 2015, while improving quality and performance. A recent study of 308 PCMHs, like Lansingburgh Family Practice, found a 62 percent reduction in acute care hospital spending and fewer ED visits.
“All you need to do is hit a button and the test is right there. I can find it through Hixny.” —Dr. Adetutu Adetona
CDPHP’s program has shown impressive results over the past eight years. EPC practices have improved in several key quality areas, including breast and colorectal cancer screenings, blood pressure control and childhood immunizations. One independent analysis found a 15 percent reduction in inpatient admissions, a 9 percent reduction in emergency room visits and an $8 per member, per month savings. The average quality score of 76.5 percent among EPC practices compares to about 60 percent in non-EPC practices.
In 2014, CDPHP realized a cost savings of $20.7 million, across all lines of business, directly related to EPC. Approximately 60 percent of that came from the commercial market, while about 20 percent was from the members of the Medicaid and Medicare markets in poorest health.
“The main thing was fewer hospitalizations,” Bennett said. “It was also fewer expensive drugs, fewer unnecessary high-tech images and lower ED use.”
Member satisfaction has risen, too. Earlier this year, J.D. Power and Associates recognized CDPHP as having the highest member satisfaction of any commercial health plan in New York. The May findings concluded that “coordination of care among healthcare providers is the single most important criteria influencing member satisfaction with their health plan.”
“Amidst sweeping changes in healthcare delivery and payment models, our data is showing that the one thing consumers value most is clear-cut, easy access to doctors and other healthcare providers,” said Valerie Monet, Senior Director of U.S. Insurance Operations at J.D. Power. “These findings set the stage for the future of healthcare, in which close coordination among health plans and providers reduces friction points for members.”
CDPHP Efforts Paid Off
EPC practices that successfully transformed to a value-based model have not only received higher pay than under the fee-for-service model, but they’ve shared in the cost savings. In 2016, CDPHP handed out $3.1 million in bonuses to EPC participants in the Capital District and beyond.
The transformation process hasn’t been simple, though. It requires a change in workflow many providers are reluctant to pursue. It involves spending more time with high-need patients and leaving slots open, so these patients don’t rely on urgent care or the ED. It requires comfort using an EHR. According to Bennett, it means cutting back on the once-uniform practice of having lunch with a drug company representative to hear them pitch their product. He says, today, successful value-based practices spend time reviewing cases and discussing patient needs as a staff. On average, Bennett believes it takes a practice one and a half years to work successfully within the EPC model.

“It’s about standing at the base of the mountain saying, ‘I will get to the top—and today I’ll take the first step,’” he said. “In taking those steps, our EPC physicians, with our help, have reached the summit and effected positive change.”
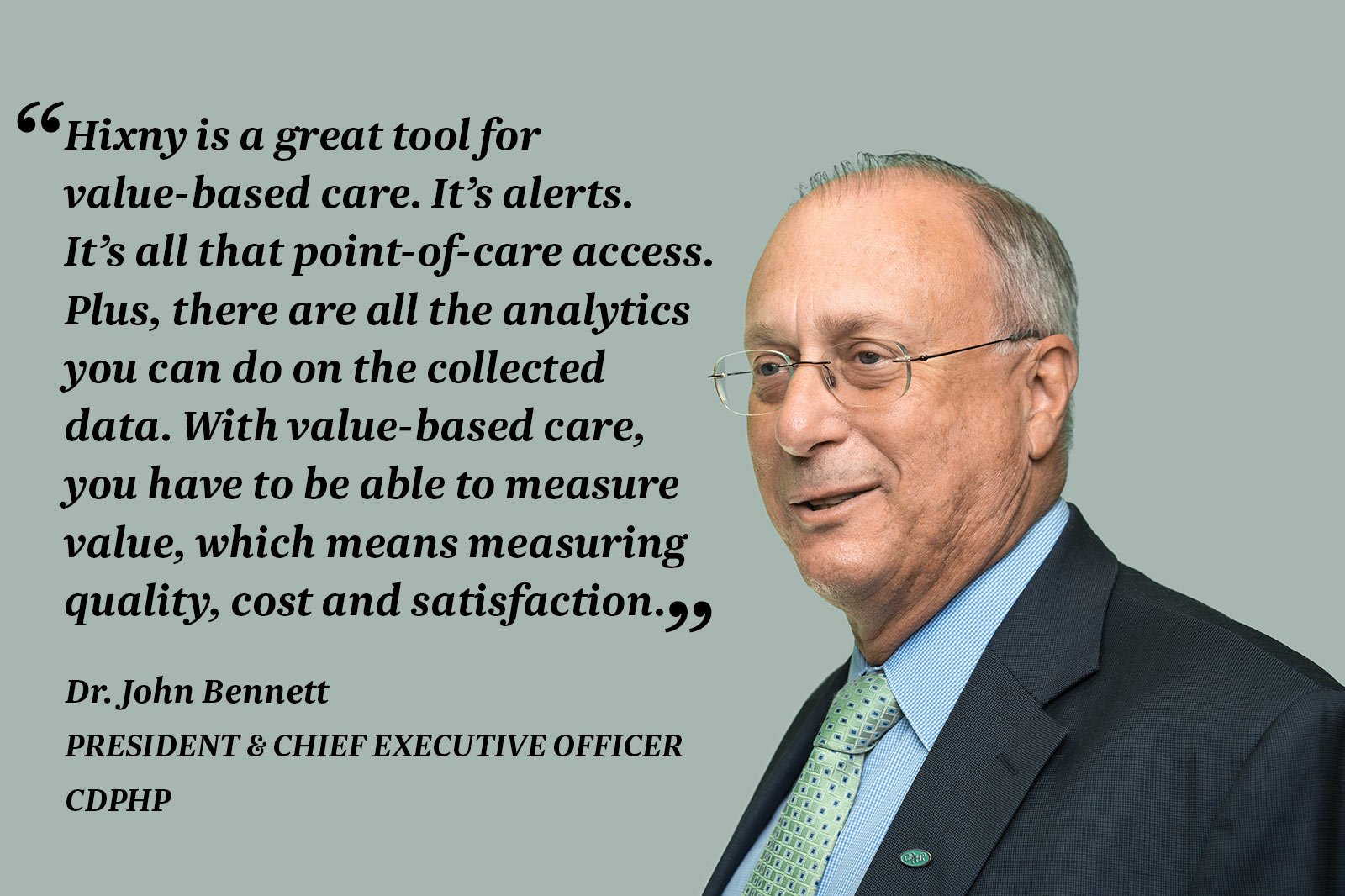
Bennett said most patients expect their primary care provider to know when they have been to the ED or what their blood pressure was, so Hixny helps the provider meet these expectations. “Hixny is a great tool for value-based care. It’s alerts. It’s all that point-of-care access. Plus, there are all the analytics you can do on the collected data. With value-based care, you have to be able to measure value, which means measuring quality, cost and satisfaction. And you need data.”
“This understanding for the need and value of data through electronic health records is one of the main reasons CDPHP has always been and remains committed to Hixny and our mission,” said McKinney.
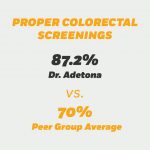
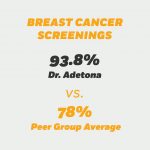
Data is where Adetona shines. CDPHP monitors 18 metrics. In her practice, 87.2 percent of appropriate patients have had a colorectal screening, above the peer-group average of 70 percent and above CDPHP’s 2018 goal of 80 percent. Her patients receive appropriate breast cancer screenings at a rate of 93.8 percent, compared to a peer group average of 78 percent. Her patients’ 96.3 percent rate on three diabetes measures towers over a peer group average of 56.7 percent.
Adetona utilizes Hixny to search for records when meeting with patients and asking if they have had the proper screenings. Often, she says, her patients are not sure if they have had the screenings or when. By accessing the Hixny record she can confirm the status, and, when needed, order the proper screening. Adetona said she understands the fears others may have when it comes to value-based-care, but she encourages them to get on board. “I have been in their position,” she said. “But you have to embrace it. Would I do it again? Yes, I would and I would have done it sooner.”